NHS executives should be regulated in a similar way to medical practitioners, the paediatrician who first raised the alarm on Lucy Letby has said. Dr Stephen Brearey said the behaviour and accountability of senior officials within the health service “absolutely” needed to be regulated. Letby is a neonatal nurse found guilty of murdering seven babies between 2015 and 2016.
“Doctors and nurses all have the regulatory bodies that we have to answer to, and quite often we’ll see senior managers who have no apparent accountability for what they do in our trusts and then move to other trusts,” Brearey told the BBC. He claimed senior staff at the Countess of Chester Hospital, where the murders took place, were worried about reputational damage to the organisation. He said that instead of acting on his warnings, he and his colleagues were made to feel under attack.
Independent inquiry
Last week the government ordered an independent inquiry into the circumstances behind the murders and attempted murders of the babies, following the guilty verdict in Letby’s trial. Launched to ensure vital lessons are learned and to provide answers to the parents and families affected, the inquiry will investigate the wider circumstances around what happened at the hospital, including the handling of concerns and governance. It will also look at what actions were taken by regulators and the wider National Health Service (NHS), the government has said.
“I would like to send my deepest sympathy to all the parents and families impacted by this horrendous case,” Health and Social Care Secretary Steve Barclay said. “This inquiry will seek to ensure the parents and families impacted get the answers they need. I am determined their voices are heard, and they are involved in shaping the scope of the inquiry should they wish to do so.”
The case has sent shockwaves through the healthcare community and the wider public. As investigations and legal proceedings continue, the case has sparked important conversations about patient safety, healthcare regulations, and the need for reforms within the UK’s NHS. Our regular columnist Carroll Barry-Walsh, a specialist lawyer and investigator, has published her own blunt assessment.
Patient welfare
Staffing levels and workloads have long been points of concern within the NHS. The case has reignited discussions about the pressures faced by healthcare professionals and the potential impact on patient care. Hospitals may consider reviewing nurse-to-patient ratios, workload distribution, and adequate rest periods to prevent burnout and maintain the highest standards of care.
The tragedy has also prompted a renewed commitment to ensuring that patient welfare is paramount in all healthcare settings. Hospitals and medical facilities are likely to reevaluate and reinforce their safety protocols, training, and oversight mechanisms to prevent similar incidents in the future.
Regulatory gaps
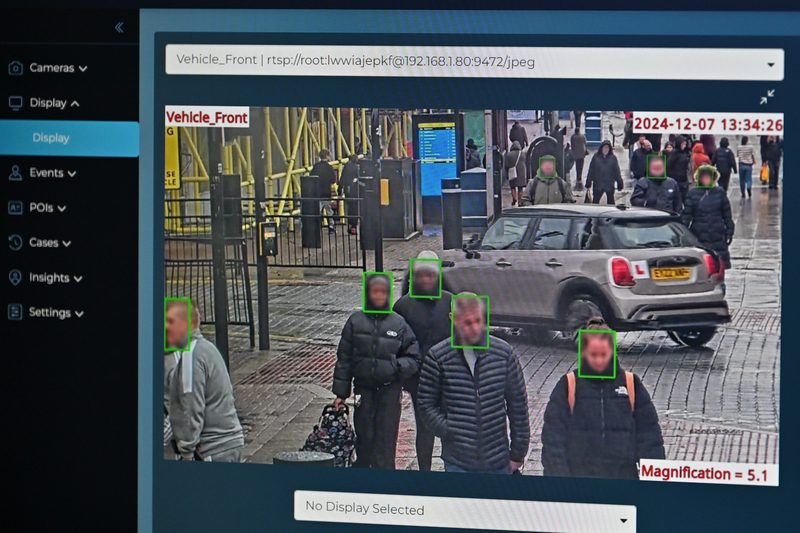
There are clear gaps in regulatory oversight within the healthcare sector. There may be calls for stricter adherence to protocols, more comprehensive monitoring of medical practices, and improved reporting mechanisms for concerns related to patient safety. Regulatory bodies may collaborate with healthcare institutions to ensure compliance with guidelines and best practices.
The case could also lead to a modernization of the NHS and how it handles data, with more focus on technological solutions that facilitate real-time data collection, analysis, and communication among medical teams, contributing to more accurate diagnoses and safer patient care.
The Letby case underscores the significance of cultivating a culture of transparency, accountability, and open communication within healthcare organizations. Hospitals may implement initiatives that encourage staff to report concerns without fear of reprisal, fostering an environment where mistakes can be identified and addressed promptly.