Private equity’s growing presence in American healthcare has long walked a tightrope between efficiency and intrusion. What once made the sector an appealing target – stable revenue streams, fragmented markets, and regulatory nuance – is now drawing increasing scrutiny.
But while federal policymakers once led the charge, today’s spotlight has shifted. As Washington’s enforcement posture turns ambivalent, the burden of oversight is migrating to statehouses. A new patchwork of laws, ranging from transaction reviews to practice ownership limits, is emerging to fill the void.
And the federal approach to PE in healthcare has grown notably less aggressive.
While 2024 brought a flurry of inquiries, most prominently, the FTC and DOJ’s joint examination of PE-backed consolidation, the momentum has waned. Proposed legislation such as the Health Over Wealth Act has stalled, and the regulatory tone has softened.
Executive orders issued in early 2025 now require agencies to pare down rules and curtail enforcement, effectively narrowing the scope of federal oversight. With FDA leadership changes and the FTC’s enforcement capacity hamstrung, the federal landscape appears less a barrier to PE than an open question. For investors, reduced compliance burdens offer short-term relief, but at the cost of predictability and institutional clarity. The real regulatory energy, increasingly, lies elsewhere.
PE’s new regulatory reckoning
As federal enforcement oscillates between ambition and inertia, state governments are assembling their own toolkit to tame private equity’s advance into healthcare. Once a matter of licensure and insurance, state healthcare policy has matured into a battleground for structural market reform.
Across the country, regulators and legislators are responding to mounting concern that investor-driven consolidation could strain local systems, inflate costs, and degrade care quality. Their response is neither ideological nor uniform, but it is coordinated, deliberate, and growing. From notification regimes to corporate practice doctrines and employment protections, states are crafting a web of legal friction that private equity firms can no longer afford to ignore.
Mini-HSR laws
The most visible, and rapidly expanding, front in this state-level campaign is the rise of so-called Mini-HSR”laws, state-specific transaction reporting statutes modeled on the federal Hart-Scott-Rodino Act. Once confined to hospital mergers, these laws have undergone a second wave of expansion, extending into areas once considered too granular for state interference.
Today, at least 15 states require advance notice of healthcare acquisitions, particularly those involving private equity, with some regimes enabling authorities not just to delay but to condition or block deals entirely.
Massachusetts, for example, now mandates that any “significant equity investor” disclose financials, ownership, and management structures 60 days before closing. That information can trigger further inquiries or be leveraged in broader cost trend analyses.
Other states are following suit, not by duplicating Massachusetts’ model but by tailoring oversight to local sensitivities. California has proposed legislation that would require PE and hedge funds to submit their federal HSR filings to the state attorney general, while expanding existing state-level reporting to management service organizations (MSOs).
Connecticut has gone further still, introducing multiple bills that would require pre-closing review for PE-led hospital acquisitions, impose transparency on sale-leaseback arrangements, and even restrict REIT involvement in healthcare. These proposals reflect a growing suspicion that complex financial engineering may be eroding accountability and increasing systemic risk.
Notably, the current trend is not about adding more states to the Mini-HSR map but deepening authority where it already exists. Since December 2024, nine states, including New York, Indiana, and Vermont, have introduced proposals to expand the scope of reportable transactions, bolster the discretion of regulators to impose conditions, and tighten scrutiny on PE-backed healthcare consolidations.
In Vermont, for instance, the Green Mountain Care Board would receive 180-day notice of major transactions and be empowered to launch extended market impact reviews. These moves suggest a quiet consensus: if federal regulators won’t move fast enough to protect patients and markets from financial overreach, states will.
Corporate practice restrictions
A more doctrinal, yet equally potent, strand of state resistance comes in the form of renewed enforcement of Corporate Practice of Medicine (CPOM) restrictions. Rooted in the idea that only licensed professionals should influence clinical decisions, these laws were once considered a regulatory relic. No longer.
States are now dusting off CPOM doctrines and applying them to contemporary investment structures like MSOs, legal vehicles PE firms often use to manage day-to-day operations while circumventing ownership restrictions on clinical entities.
Recent proposals in at least six states, California, Connecticut, Oregon, South Carolina, Vermont, and Washington, seek to sharpen these prohibitions. California’s SB 351, for instance, would explicitly bar PE-owned MSOs from controlling key functions such as hiring and firing clinicians, influencing clinical documentation, or setting billing parameters.
In Vermont, proposed legislation would prohibit equity transfer arrangements that allow clinician-owners to relinquish control to MSOs. These bills aim to pierce the corporate veil, ensuring that legal form does not obscure de facto control by financial sponsors.
The CPOM revival is especially consequential for digital health and multi-state providers. While the MSO-PC (professional corporation) model remains the gold standard for CPOM compliance, its implementation now demands surgical precision.
States are increasingly questioning whether administrative service agreements, equity transfer restriction agreements (ETRAs), and continuity planning arrangements give PE investors more than just back-office influence. In jurisdictions with aggressive enforcement, even subtle encroachments on physician autonomy can trigger allegations of unauthorized practice or illicit fee-splitting.
Compounding the challenge, CPOM laws are not uniform. Some states rely on statutory prohibitions, others on case law or informal attorney general guidance. This patchwork forces PE firms into a high-stakes compliance maze, one where a misstep can invalidate corporate structures, jeopardize licensure, and attract scrutiny from multiple regulators. As CPOM doctrine evolves, legal creativity is no longer a virtue, it is a risk factor.
Non-compete clauses
Beyond transactions and control structures, states are also zeroing in on employment practices, most notably, the use of non-compete clauses. Although the federal government’s effort to impose a blanket ban faltered in 2024, the states have carried the torch. Four states now ban non-competes outright, while more than 30 others, including Washington, D.C., impose significant restrictions.
These reforms are reshaping the labor economics of PE-backed healthcare, particularly in rural or specialty-scarce markets where talent retention was once secured contractually.
Ohio is a telling example of this shift. A bipartisan bill introduced in the state senate in early 2025 would ban nearly all forms of non-compete agreements, including those involving independent contractors and sole proprietors. The bill also bars employers from penalizing workers who leave and limits the use of forum selection or governing law clauses designed to skirt local protections. If passed, the law would place Ohio among the strictest jurisdictions in the nation, transforming a once PE-friendly state into a frontline of employment rights enforcement.
For private equity investors, these developments present a dual threat. Not only do they erode a key post-acquisition retention mechanism, but they also introduce unpredictability into deal valuation.
If seller-physicians can depart and compete immediately after a transaction, the strategic value of the asset, and the assumptions underlying exit timelines, may be upended. With non-compete laws advancing on multiple fronts, PE firms may need to shift focus from contractual enforcement to cultural retention strategies, particularly in high-stakes clinical platforms.
States step forward, again
The widening patchwork of state laws governing private equity investment in healthcare is not an isolated phenomenon, it is a harbinger. As federal agencies retreat or fracture along partisan lines, the burden of regulatory governance is shifting ever more decisively to state capitals.
For healthcare PE investors, this shift signals a permanent recalibration of compliance risk. Gone are the days when federal inaction created breathing room for creative structuring or aggressive roll-ups. Instead, firms must contend with multi-jurisdictional oversight regimes where notice periods lengthen, review thresholds shrink, and the definition of “material” becomes ever more elastic.
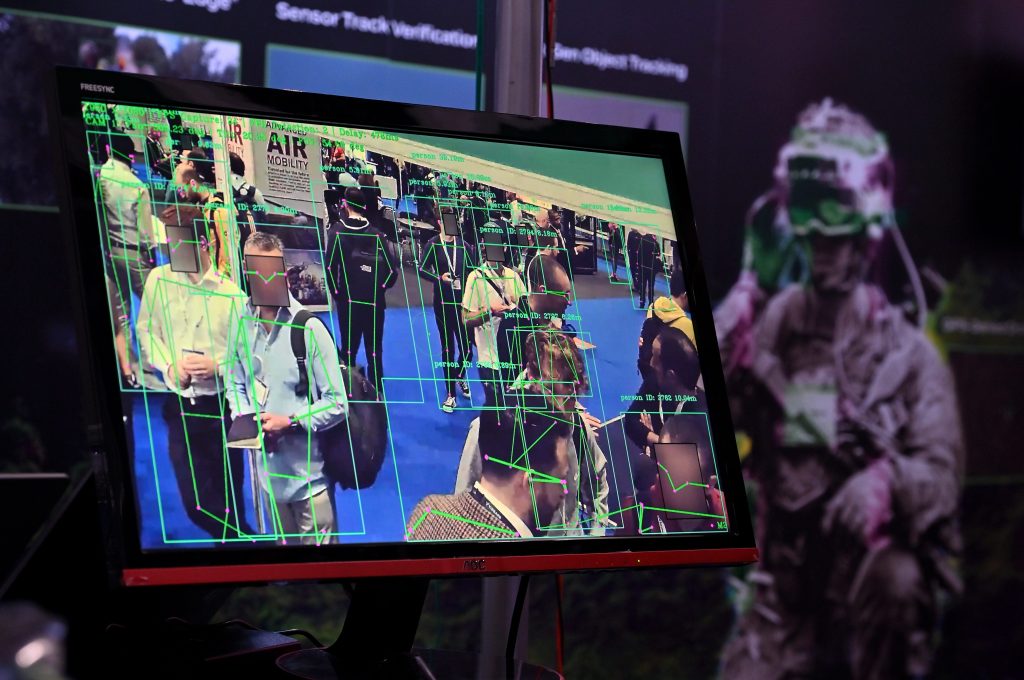
But the implications extend beyond healthcare. Climate-related mandates, AI governance, and consumer protection rules are increasingly incubated in state legislatures and enforced by state attorneys general. For private capital, the era of state capture may be giving way to an era of state constraint: one where deal strategy, risk modeling, and operational planning will depend as much on Albany and Sacramento as on Washington.